 More than 18 million Americans have symptoms of PAD, or peripheral arterial disease, which is also known as peripheral vascular disease (PVD). September is a month to honor people who battle circulatory conditions and may face limb amputation. Help us spread PAD awareness and encourage early detection.
More than 18 million Americans have symptoms of PAD, or peripheral arterial disease, which is also known as peripheral vascular disease (PVD). September is a month to honor people who battle circulatory conditions and may face limb amputation. Help us spread PAD awareness and encourage early detection.
What is PAD?
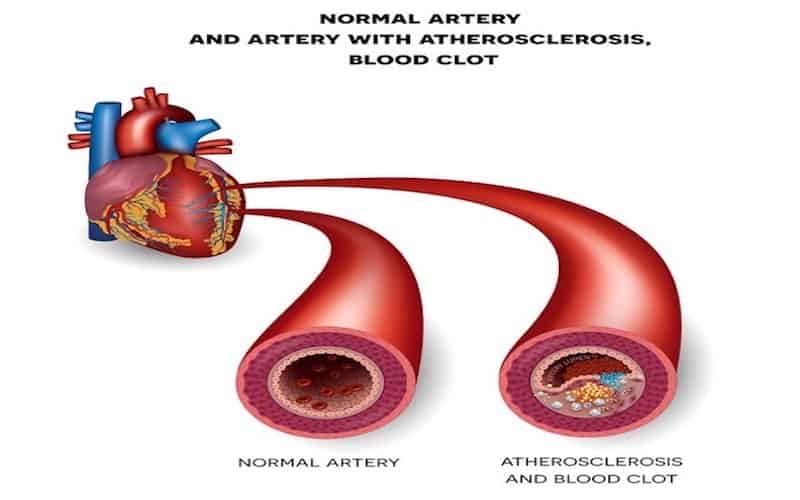
While peripheral arterial disease is a relatively common condition, many people are unaware that they have it. PAD causes limited circulation to the body, particularly the limbs, and restricts vital blood flow. PAD can also be an indication of fatty deposits in the body’s arteries, or atherosclerosis, which puts the heart and brain at risk.
What are PAD’s Symptoms?
One of the earliest symptoms of peripheral arterial disease is periodic twitching or cramping in the hands, legs, and feet that disappears after a few minutes of rest. This may also be felt in the hips, thighs, and shoulders. Over time, people with PAD may have symptoms like:
- Painful cramping, especially in the extremities and calves
- Leg and arm numbness
- A persistent feeling of cold in a foot or hand
- Sores that won’t heal
- Changes in skin color and texture, including shiny skin
- Slowed growth in body hair or nails
- Erectile dysfunction
- Sleep disruption
- Slowed pulse
- Widespread, unexplained pain
Who is a Candidate for a PAD Diagnosis?
One of the reasons for PAD Awareness Month is to bring attention to the fact that PAD can be a silent killer, and is not just an “old person’s” disease. Many people can develop peripheral arterial disease, although the most common candidates are:
- Anyone over age 65
- People over age 50 with diabetes, who smoke, or have other high-risk factors like obesity, high cholesterol, or high blood pressure
- People over age 50 with a family history of PAD or diabetes, even if they don’t have it themselves
- Adults of African-American and Hispanic ethnicity, because men and women of these backgrounds have a higher risk of developing PAD
- Adults with limb injury, radiation exposure, muscle and ligament problems, and a hereditary increased level of homocysteine – a tissue-building protein
If you have any of the risk factors described above, get checked for peripheral arterial disease – especially if you have experienced limb cramping or numbness. The symptoms can be subtle at first and early detection is key.
Why is Early Detection so Important?
Many people who are currently living with PAD have no symptoms and don’t realize they have it. Meanwhile, the disease is progressing throughout their body, doing damage along the way.
Early detection allows doctors to intervene and take potentially life-saving preventive steps, including:
- Lowering your blood pressure
- Addressing the causes of high cholesterol
- Providing wound care for persistent sores
- Preventing arterial damage
- Preventing limb amputation
How Do Doctors Diagnose PAD?
Tests for PAD are painless and noninvasive. It starts with an ankle-brachial index (ABI) test, which compares your ankle blood pressure to your arm blood pressure to see if there’s a difference.
Varied blood pressure throughout the body is one of the key indicators of peripheral arterial disease. It shows that your limbs and digits may be at risk due to restricted blood flow. A vascular specialist can use their extensive knowledge of the body’s systems to properly diagnose peripheral arterial disease and recommend the right treatment for each person.
What is the Treatment for PAD?
Treatment involves an array of therapies, from outpatient treatment at a vascular center to at-home lifestyle changes. Through medicine and therapy, you will work to minimize the risks associated with peripheral arterial disease in terms of blood pressure, cholesterol, wounds, and body-wide system health.
Your doctor will likely recommend increased physical activity and diet changes that will help you manage your PAD. Physical therapy helps many peripheral arterial disease patients. Low-impact exercises like walking and leg stretches can slowly build in intensity, under careful monitoring.
If you smoke, your doctor will recommend smoking cessation and may evaluate you for risks associated with stroke and heart attack. Smoking makes PAD symptoms worse.
Medication focuses on lowering your blood pressure, lowering your cholesterol, and preventing blood clots from forming. Peripheral arterial disease medications may work in tandem with procedures like angioplasty, stent placement, or atherectomy. These procedures are aimed at allowing blood to flow freely throughout the body.
Can PAD Be Prevented?
Although this disease is not entirely preventable, you can educate yourself about prevention and significantly lessen your risk by taking these positive steps:
Exercise regularly. Exercise is important, but consult a doctor before starting a new exercise program. Avoid long periods of sitting, especially with your legs motionless. Aim for at least 30 to 45 minutes, several times a week, of easy to moderate physical exercise.
Eat a PAD prevention diet. A diet that prevents peripheral arterial disease is the same type of diet that supports heart health and prevents obesity: Eat lots of green vegetables and avoid high-cholesterol foods. Avoid sugar and alcohol. Eat a diet that is low in saturated and trans fats.
Manage diabetes. If you have diabetes, it is important to manage it carefully to limit potential damage, like losing a limb.
Don’t smoke. Smoking increases your chance of developing peripheral arterial disease by 2 to 6 times and worsens your symptoms significantly.
Schedule regular checkups. This disease is often caught during routine checkups or an early detection screening at a vascular specialist. Alert your doctor to any changes in your health, like persistent sores, pain, numbness, or cramps.
A Proactive Approach to PAD
If you are concerned about peripheral arterial disease, connect with the specialists at Maryland Vascular Specialists for an evaluation. Early detection can prevent loss of limbs and life, and keep you on the right track to long-term health.