- Arteriogram (or angiogram), an x-ray of the blood vessels with contrast dye
- Duplex ultrasound, a test that checks blood flow in the renal veins and arteries
- Renography, which checks kidney structure and function
- Magnetic resonance angiography (MRA), a way to observe the blood vessels
Treatment for renal vascular disease depends on how your body has been affected by the disease. Treatment may include:
- Blood pressure lowering medication
- Cholesterol-lowering medication
- Diabetes-related medication
- Clot-busting medication
- Anticoagulant medication
- An endovascular procedure like angioplasty, which opens the renal artery
- Surgery to bypass a blocked renal artery
- Surgery to remove a clot
In some cases, an approach of careful watching and waiting may be recommended by your doctor. Your doctor may also recommend lifestyle changes, like diet changes, avoiding foods high in fat and salt, and increasing moderate exercise.
{,}show_first{:}{|}tab_name{:}What Are The Risk Factors?{,}tab_content{:}Certain people are at a higher risk of renal vascular disease due to a combination of genetic and lifestyle factors. These factors include:
- Being female
- Older age
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
- Injury to the body, including surgery
- Infections
- Inflammation, perhaps from underlying disease
- Tumors
- Pregnancy
- Certain medications
- Birth defects that may or may not be obvious
With care from a vascular specialist or surgeon, you can limit further damage to the kidneys. Vascular care helps prevent permanent damage and preserves your body-wide health.
Remember, renal vascular disease can occur with no symptoms or an array of symptoms that are similar to other conditions. For a proper diagnosis, schedule a consultation with Maryland Vascular Specialists.
{,}show_first{:} )Renal Vascular Disease
Overview Of Renal Vascular Disease
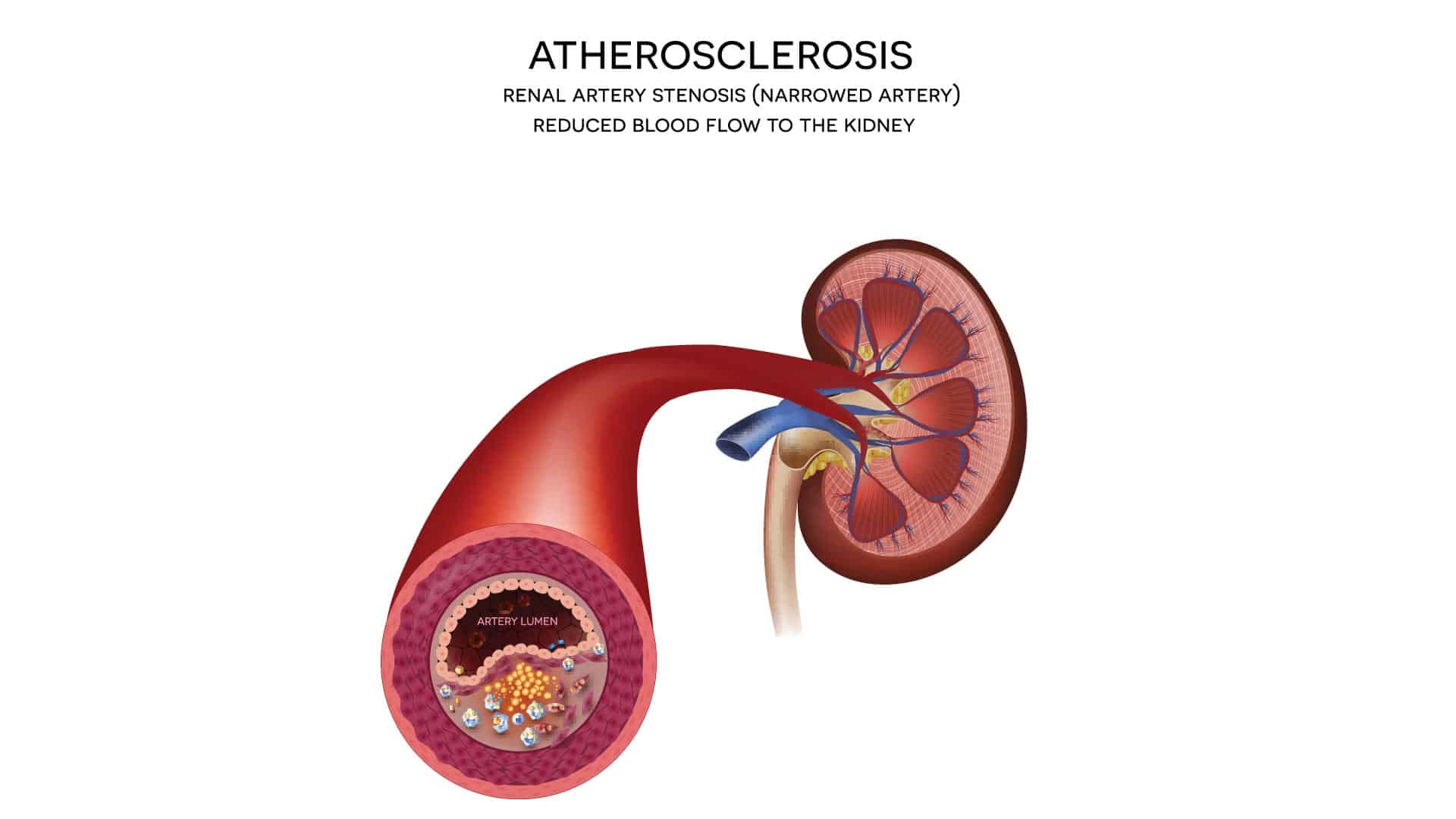
When someone has renal vascular disease, their blood isn’t flowing normally to and from the kidneys. This can cause health complications including high blood pressure, kidney damage, and kidney failure.
Renal vascular disease involves the hormone renin, which raises blood pressure. When you have decreased blood flow to the kidneys due to renal vascular disease, you may have too much renin in the blood which results in excessively high blood pressure.
Renal vascular disease is related to the following conditions:
- Renal artery stenosis (RAS), a narrowing of the artery to the kidneys
- Renal artery thrombosis, a blood clot in the artery to the kidney
- Renal vein thrombosis, a clot in a vein to the kidney
- Renal artery aneurysm, from a weak area in the wall of the artery to the kidney
- Atheroembolic renal disease, from plaque breaking off and moving through the blood
Symptoms Of Renal Vascular Disease
A person with renal vascular disease may experience a wide array of symptoms, depending on how it is affecting their body. Any of the following symptoms can be an indicator of renal vascular disease:
- Persistent high blood pressure, even despite medication
- Blood with high urea, a waste byproduct of the kidneys
- Sudden-onset side pain
- Side and hip pain and tenderness
- Belly pain
- High and/or persistent fever
- Blood in the urine
- Nausea and vomiting
- Skin Lesions
- Red or purple discoloration of the skin
- Discoloration in the toes and feet
- Diarrhea
- Mental confusion
- Unexplained weight loss
- Muscle aches
- Spasms in the body, especially the hips and flank
- Soreness in the kidney area
- Sudden or unexplained kidney failure
It is important to note that some people with renal vascular disease have no symptoms. These patients are often diagnosed through routine medical screenings and checkups.
Your doctor at Maryland Vascular Specialists will work with your general practitioner or other doctors to create a complete health history. In addition to doing a physical exam, your doctor may perform tests including:
- Arteriogram (or angiogram), an x-ray of the blood vessels with contrast dye
- Duplex ultrasound, a test that checks blood flow in the renal veins and arteries
- Renography, which checks kidney structure and function
- Magnetic resonance angiography (MRA), a way to observe the blood vessels
Treatment for renal vascular disease depends on how your body has been affected by the disease. Treatment may include:
- Blood pressure lowering medication
- Cholesterol-lowering medication
- Diabetes-related medication
- Clot-busting medication
- Anticoagulant medication
- An endovascular procedure like angioplasty, which opens the renal artery
- Surgery to bypass a blocked renal artery
- Surgery to remove a clot
In some cases, an approach of careful watching and waiting may be recommended by your doctor. Your doctor may also recommend lifestyle changes, like diet changes, avoiding foods high in fat and salt, and increasing moderate exercise.
Certain people are at a higher risk of renal vascular disease due to a combination of genetic and lifestyle factors. These factors include:
- Being female
- Older age
- High blood pressure
- High cholesterol
- Smoking
- Diabetes
- Injury to the body, including surgery
- Infections
- Inflammation, perhaps from underlying disease
- Tumors
- Pregnancy
- Certain medications
- Birth defects that may or may not be obvious
With care from a vascular specialist or surgeon, you can limit further damage to the kidneys. Vascular care helps prevent permanent damage and preserves your body-wide health.
Remember, renal vascular disease can occur with no symptoms or an array of symptoms that are similar to other conditions. For a proper diagnosis, schedule a consultation with Maryland Vascular Specialists.