What does the MACRA Final Rule mean for practitioners?
The Centers for Medicare and Medicaid Services released the final rule for the Medicare Access and CHIP Reauthorization Act, a landmark payment system that modernizes the payments for Medicare physician fees. These rules became effective in January 2017.
The following is a brief summary of this massive new law on a very basic level. Over the next few months, we will share more information.
The Basics: 8 Things Practitioners Need to Know About the MACRA Final Rule
1. What is the MACRA Final Rule?
The rule finalizes MACRA’s Quality Payment Program. This is CMS’s aim to reduce the administrative burden on physicians, so they can focus on care improvement, promote adoption of value-based care, and smooth the transition to these new models of care.
This attempt to modernize the Medicare physician payment system offers a more streamlined and effective approach to supporting high-quality patient care.
2. Who qualifies for the Quality Payment Program?
Physicians, physician assistants, nurse practitioners, clinical nurse specialists, and certified registered nurse anesthetists who bill Medicare more than $30,000 a year or provide care for at least 100 Medicare patients qualify for MACRA. Providers who are new to Medicare in 2017, are not required to participate until 2018.
3. When does the Quality Payment Program start?
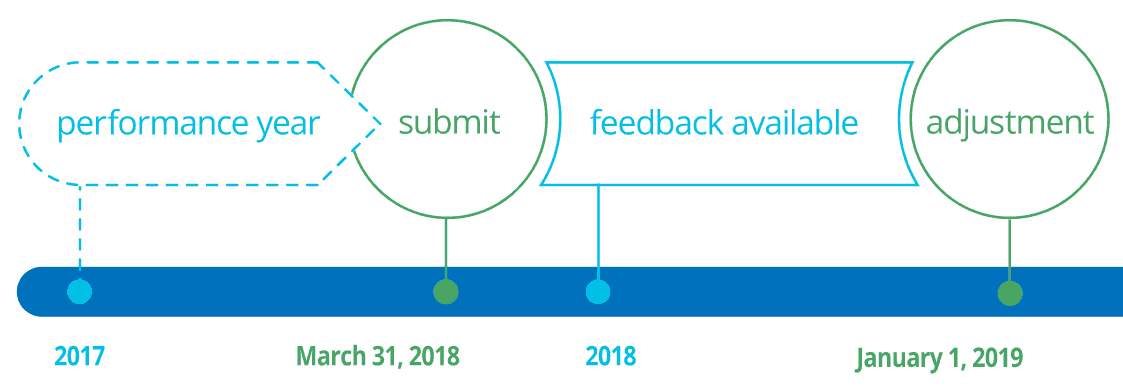
Providers who are ready to start collecting performance data can begin as early as Jan. 1, 2017. However, CMS is offering providers the option to start anytime between Jan. 1 and Oct. 2. No matter when providers begin collecting data, it is due to CMS by March 31, 2018. The data collected in the first performance year will determine payment adjustments beginning Jan. 1, 2019.
4. What options are there for participation?
The MACRA QPP creates two pathways for Medicare-participating physicians:
- MIPS – designed for providers in traditional, fee-for-service Medicare.
- Advanced Alternative Payment Models (Advanced APM) – designed for providers who participate in specific value-based care models.
5. What is MIPS and how has it changed from the proposed rule?
MIPS rolls together three legacy CMS programs: Meaningful Use, the Physician Quality Reporting System and the Value-Based Payment Modifier. Physicians will earn payment adjustments based on performance in four categories linked to quality and value that will be similar to the previous programs. Payment adjustments in the first year will be neutral, positive or negative up to 4 percent. This grows to 9 percent by 2022. CMS has agreed to implement this rule on a gradual ramp to full participation, so physicians may pick their pace between the following four options in 2017.
- No participation and an automatic 4 percent negative payment adjustment.
- Submission of a minimum amount of data — i.e. one quality measure — and a neutral payment adjustment.
- Submission of 90 days of data for a potential small positive payment adjustment or a neutral adjustment.
- Submission of a full year of data for the potential to earn a moderate positive payment adjustment.
6. What qualifies as an advanced APM?
Physicians are able to earn a five (5) percent lump-sum incentive payment each year from 2019 through 2024 and avoid MIPS reporting requirements and payment adjustments by participating in the advanced APM. To qualify, advanced APMs must meet three requirements: 1) use certified EHR technology, 2) base payments on quality measures comparable to MIPS and 3) require providers to bear more than nominal risk. CMS must approve all advanced APMs. The final rule identifies the following as advanced APMs for 2017:
- Comprehensive ESRD Care Model (LDO and non-LDO two-sided risk arrangements)
- Comprehensive Primary Care Plus Model
- Medicare Shared Savings Program Tracks 2 and 3
- Next Generation ACO Model
Later in 2017 or 2018, CMS plans to create additional pathways for participating in the advanced APM track, including:
- New accountable care organization Track 1+ model
- Comprehensive Care for Joint Replacement
- Medicare Diabetes Prevention Program
7. How can small practices participate and qualify for MACRA Quality Payment Program incentives?

CMS’ adjustments to the proposed rule help small, independent practices participate. Practices, which fall below the requirements of at least $30,000 Medicare Part B charges or 100 Medicare patients, are exempt from participating in 2017. Additionally, CMS is offering small practices and solo physicians to join together in virtual groups and submit combined MIPS data. The final rule allows $20 million a year for five years for training and education of physicians in practices of 15 or fewer and those who work in underserved areas. View the CMS Support for Small Practices fact sheet HERE.
8. How is the final rule more streamlined?
CMS highlighted five key changes that reflect this effort to streamline Medicare reforms:
-
- 1. Offering more flexible options in the first year
-
- 2. Providing adjustment of the low-volume threshold for small practices
-
- 3. Establishing the advanced APM as a standard to promote participation in value-based care models
-
- 4. Simplifying “all-or-nothing” EHR requirements, and
-
- 5. Supporting the medical home model to promote care coordination.
Where may I learn more?
Click HERE for more educational resources and details about the MACRA Quality Payment Program. CMS will also answer any questions you may have by email (send to QPP@cms.hhs.gov) and phone (call 1-866-288-8292).
